STI Information
- HIV
- Gonorrhea
- Chlamydia
- Genital Herpes
- Syphilis
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Human Papillomavirus (HPV)
- Urethritis, Mycoplasma Genitalium
- Bacterial Vaginosis
- Scabies
- Pelvic Inflammatory Disease
- Pediculosis (Lice)
- Trichomoniasis
HIV stands for human immunodeficiency virus. It is the virus that can lead to acquired immunodeficiency syndrome, or AIDS. Unlike some other viruses, the human body cannot get rid of HIV. That means that once you have HIV, you have it for life.
No safe and effective cure currently exists, but scientists are working hard to find one, and remain hopeful. Meanwhile, with proper medical care, HIV can be controlled. Treatment for HIV is often called antiretroviral therapy or ART. It can dramatically prolong the lives of many people infected with HIV and lower their chance of infecting others. Before the introduction of ART in the mid-1990s, people with HIV could progress to AIDS in just a few years. Today, someone diagnosed with HIV and treated before the disease is far advanced can have a nearly normal life expectancy.
HIV affects specific cells of the immune system, called CD4 cells, or T cells. Over time, HIV can destroy so many of these cells that the body can’t fight off infections and disease. When this happens, HIV infection leads to AIDS.Where did HIV come from?
What are the stages of HIV?
HIV disease has a well-documented progression. Untreated, HIV is almost universally fatal because it eventually overwhelms the immune system—resulting in acquired immunodeficiency syndrome (AIDS). HIV treatment helps people at all stages of the disease, and treatment can slow or prevent progression from one stage to the next.
A person can transmit HIV to others during any of these stages:
Acute infection: Within 2 to 4 weeks after infection with HIV, you may feel sick with flu-like symptoms. This is called acute retroviral syndrome (ARS) or primary HIV infection, and it’s the body’s natural response to the HIV infection. (Not everyone develops ARS, however—and some people may have no symptoms.)
During this period of infection, large amounts of HIV are being produced in your body. The virus uses important immune system cells called CD4 cells to make copies of itself and destroys these cells in the process. Because of this, the CD4 count can fall, quickly.
Your ability to spread HIV is highest during this stage because the amount of virus in the blood is very high.
Eventually, your immune response will begin to bring the amount of virus in your body back down to a stable level. At this point, your CD4 count will then begin to increase, but it may not return to pre-infection levels.
Clinical latency (inactivity or dormancy): This period is sometimes called asymptomatic HIV infection or chronic HIV infection. During this phase, HIV is still active, but reproduces at very low levels. You may not have any symptoms or get sick during this time. People who are on antiretroviral therapy (ART) may live with clinical latency for several decades. For people who are not on ART, this period can last up to a decade, but some may progress through this phase faster. It is important to remember that you are still able to transmit HIV to others during this phase even if you are treated with ART, although ART greatly reduces the risk. Toward the middle and end of this period, your viral load begins to rise and your CD4 cell count begins to drop. As this happens, you may begin to have symptoms of HIV infection as your immune system becomes too weak to protect you .
AIDS (acquired immunodeficiency syndrome): This is the stage of infection that occurs when your immune system is badly damaged and you become vulnerable to infections and infection-related cancers called opportunistic illnesses. When the number of your CD4 cells falls below 200 cells per cubic millimeter of blood (200 cells/mm3), you are considered to have progressed to AIDS. (Normal CD4 counts are between 500 and 1,600 cells/mm3.) You can also be diagnosed with AIDS if you develop one or more opportunistic illnesses, regardless of your CD4 count. Without treatment, people who are diagnosed with AIDS typically survive about 3 years. Once someone has a dangerous opportunistic illness, life expectancy without treatment falls to about 1 year. People with AIDS need medical treatment to prevent death.collapsed
 Scientists identified a type of chimpanzee in West Africa as the source of HIV infection in humans. They believe that the chimpanzee version of the immunodeficiency virus (called simian immunodeficiency virus, or SIV) most likely was transmitted to humans and mutated into HIV when humans hunted these chimpanzees for meat and came into contact with their infected blood. Studies show that HIV may have jumped from apes to humans as far back as the late 1800s. Over decades, the virus slowly spread across Africa and later into other parts of the world. We know that the virus has existed in the United States since at least the mid- to late 1970s.How can I tell if I’m infected with HIV? collapsed
Scientists identified a type of chimpanzee in West Africa as the source of HIV infection in humans. They believe that the chimpanzee version of the immunodeficiency virus (called simian immunodeficiency virus, or SIV) most likely was transmitted to humans and mutated into HIV when humans hunted these chimpanzees for meat and came into contact with their infected blood. Studies show that HIV may have jumped from apes to humans as far back as the late 1800s. Over decades, the virus slowly spread across Africa and later into other parts of the world. We know that the virus has existed in the United States since at least the mid- to late 1970s.How can I tell if I’m infected with HIV? collapsed
The only way to know if you are infected with HIV is to be tested. You cannot rely on symptoms to know whether you have HIV. Many people who are infected with HIV do not have any symptoms at all for 10 years or more. Some people who are infected with HIV report having flu-like symptoms (often described as “the worst flu ever”) 2 to 4 weeks after exposure. Symptoms can include:
- Fever
- Enlarged lymph nodes
- Sore throat
- Rash
These symptoms can last anywhere from a few days to several weeks. During this time, HIV infection may not show up on an HIV test, but people who have it are highly infectious and can spread the infection to others.
However, you should not assume you have HIV if you have any of these symptoms. Each of these symptoms can be caused by other illnesses. Again, the only way to determine whether you are infected is to be tested for HIV infection. For information on where to find an HIV testing site,
- Visit https://gettested.cdc.gov/ and enter your ZIP code.
- Text your ZIP code to KNOWIT (566948), and you will receive a text back with a testing site near you.
- Call the CDC to ask for free testing sites in your area.
These resources are confidential. You can also ask your health care provider to give you an HIV test.
Two types of home testing kits are available in most drugstores or pharmacies: one involves pricking your finger for a blood sample, sending the sample to a laboratory, then phoning in for results. The other involves getting a swab of fluid from your mouth, using the kit to test it, and reading the results in 20 minutes. Confidential counseling and referrals for treatment are available with both kinds of home tests.
If you test positive for HIV, you should see your doctor as soon as possible to begin treatment.Is there a cure for HIV?
For most people, the answer is no. Most reports of a cure involve HIV-infected people who needed treatment for a cancer that would have killed them otherwise. But these treatments are very risky, even life-threatening, and are used only when the HIV-infected people would have died without them. Antiretroviral therapy (ART), however, can dramatically prolong the lives of many people infected with HIV and lower their chance of infecting others. It is important that people get tested for HIV and know that they
What is gonorrhea?
Gonorrhea is a sexually transmitted disease (STD) that can infect both men and women. It can cause infections in the genitals, rectum, and throat. It is a very common infection, especially among young people ages 15-24 years.
How is gonorrhea spread?
You can get gonorrhea by having vaginal, anal, or oral sex with someone who has gonorrhea. A pregnant woman(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm) with gonorrhea can give the infection to her baby during childbirth.
How can I reduce my risk of getting gonorrhea?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting gonorrhea:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
Am I at risk for gonorrhea?
Any sexually active person can get gonorrhea through unprotected vaginal, anal, or oral sex.
If you are sexually active, have an honest and open talk with your health care provider and ask whether you should be tested for gonorrhea or other STDs. If you are a sexually active man who is gay, bisexual, or who has sex with men, you should be tested for gonorrhea every year. If you are a sexually active women younger than 25 years or an older women with risk factors such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection, you should be tested for gonorrhea every year.
I'm pregnant. How does gonorrhea affect my baby?
If you are pregnant(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm) and have gonorrhea, you can give the infection to your baby during delivery. This can cause serious health problems for your baby. If you are pregnant, it is important that you talk to your health care provider so that you get the correct examination, testing, and treatment, as necessary. Treating gonorrhea as soon as possible will make health complications for your baby less likely.
How do I know if I have gonorrhea?
Some men with gonorrhea may have no symptoms at all. However, men who do have symptoms, may have:
- A burning sensation when urinating;
- A white, yellow, or green discharge from the penis;
- Painful or swollen testicles (although this is less common).
Most women with gonorrhea do not have any symptoms. Even when a woman has symptoms, they are often mild and can be mistaken for a bladder or vaginal infection. Women with gonorrhea are at risk of developing serious complications from the infection, even if they don’t have any symptoms.
Symptoms in women can include:
- Painful or burning sensation when urinating;
- Increased vaginal discharge;
- Vaginal bleeding between periods.
Rectal infections may either cause no symptoms or cause symptoms in both men and women that may include:
- Discharge;
- Anal itching;
- Soreness;
- Bleeding;
- Painful bowel movements.
You should be examined by your doctor if you notice any of these symptoms or if your partner has an STD or symptoms of an STD, such as an unusual sore, a smelly discharge, burning when urinating, or bleeding between periods.
How will my doctor know if I have gonorrhea?
Most of the time, urine can be used to test for gonorrhea. However, if you have had oral and/or anal sex, swabs may be used to collect samples from your throat and/or rectum. In some cases, a swab may be used to collect a sample from a man’s urethra (urine canal) or a woman’s cervix (opening to the womb).
Can gonorrhea be cured?
Yes, gonorrhea can be cured with the right treatment(http://www.cdc.gov/std/gonorrhea/treatment.htm). It is important that you take all of the medication your doctor prescribes to cure your infection. Medication for gonorrhea should not be shared with anyone. Although medication will stop the infection, it will not undo any permanent damage caused by the disease.
It is becoming harder to treat some gonorrhea, as drug-resistant strains of gonorrhea(http://www.cdc.gov/std/gonorrhea/arg/default.htm) are increasing. If your symptoms continue for more than a few days after receiving treatment, you should return to a health care provider to be checked again.
I was treated for gonorrhea. When can I have sex again?
You should wait seven days after finishing all medications before having sex. To avoid getting infected with gonorrhea again or spreading gonorrhea to your partner(s), you and your sex partner(s) should avoid having sex until you have each completed treatment. If you’ve had gonorrhea and took medicine in the past, you can still get infected again if you have unprotected sex with a person who has gonorrhea.
What happens if I don’t get treated?
Untreated gonorrhea can cause serious and permanent health problems in both women and men.
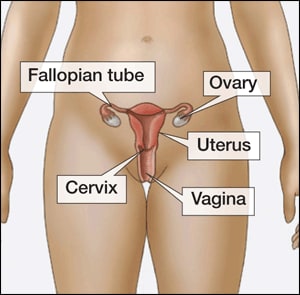
In women, untreated gonorrhea can cause pelvic inflammatory disease (PID)(http://www.cdc.gov/std/pid/stdfact-pid.htm). Some of the complications of PID are
- Formation of scar tissue that blocks fallopian tubes;
- Ectopic pregnancy (pregnancy outside the womb);
- Infertility (inability to get pregnant);
- Long-term pelvic/abdominal pain.
In men, gonorrhea can cause a painful condition in the tubes attached to the testicles. In rare cases, this may cause a man to be sterile, or prevent him from being able to father a child.
Rarely, untreated gonorrhea can also spread to your blood or joints. This condition can be life-threatening.
Untreated gonorrhea may also increase your chances of getting or giving HIV(http://www.cdc.gov/std/hiv/stdfact-std-hiv.htm) – the virus that causes AIDS.
What is chlamydia?
Chlamydia(http://www.cdc.gov/std/chlamydia/default.htm) is a common STD that can infect both men and women. It can cause serious, permanent damage to a woman's reproductive system, making it difficult or impossible for her to get pregnant later on. Chlamydia can also cause a potentially fatal ectopic pregnancy (pregnancy that occurs outside the womb).
How is chlamydia spread?
You can get chlamydia by having vaginal, anal, or oral sex with someone who has chlamydia.
If your sex partner is male you can still get chlamydia even if he does not ejaculate (cum).
If you’ve had chlamydia and were treated in the past, you can still get infected again if you have unprotected sex with someone who has chlamydia.
If you are pregnant, you can give chlamydia to your baby during childbirth(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm).
How can I reduce my risk of getting chlamydia?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
Am I at risk for chlamydia?
Anyone who has sex can get chlamydia through unprotected vaginal, anal, or oral sex. However, sexually active young people are at a higher risk of getting chlamydia. This is due to behaviors and biological factors common among young people. Gay, bisexual, and other men who have sex with men are also at risk since chlamydia can be spread through oral and anal sex.
Have an honest and open talk with your health care provider and ask whether you should be tested for chlamydia or other STDs. If you are a sexually active woman younger than 25 years, or an older woman with risk factors such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection, you should get a test for chlamydia every year. Gay, bisexual, and men who have sex with men; as well as pregnant women should also be tested for chlamydia(http://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm).
I'm pregnant. How does chlamydia affect my baby?
If you are pregnant and have chlamydia, you can pass the infection to your baby during delivery. This could cause an eye infection or pneumonia in your newborn. Having chlamydia may also make it more likely to deliver your baby too early.
If you are pregnant, you should be tested for chlamydia at your first prenatal visit. Testing and treatment are the best ways to prevent health problems.
How do I know if I have chlamydia?
 Most people who have chlamydia have no symptoms. If you do have symptoms, they may not appear until several weeks after you have sex with an infected partner. Even when chlamydia causes no symptoms, it can damage your reproductive system.
Most people who have chlamydia have no symptoms. If you do have symptoms, they may not appear until several weeks after you have sex with an infected partner. Even when chlamydia causes no symptoms, it can damage your reproductive system.
Women with symptoms may notice
- An abnormal vaginal discharge;
- A burning sensation when urinating.
Symptoms in men can include
- A discharge from their penis;
- A burning sensation when urinating;
- Pain and swelling in one or both testicles (although this is less common).
Men and women can also get infected with chlamydia in their rectum, either by having receptive anal sex, or by spread from another infected site (such as the vagina). While these infections often cause no symptoms, they can cause
- Rectal pain;
- Discharge;
- Bleeding.
You should be examined by your doctor if you notice any of these symptoms or if your partner has an STD or symptoms of an STD, such as an unusual sore, a smelly discharge, burning when urinating, or bleeding between periods.
How will my doctor know if I have chlamydia?
There are laboratory tests to diagnose chlamydia. Your health care provider may ask you to provide a urine sample or may use (or ask you to use) a cotton swab to get a sample from your vagina to test for chlamydia.
Can chlamydia be cured?
Yes, chlamydia can be cured with the right treatment. It is important that you take all of the medication your doctor prescribes to cure your infection. When taken properly it will stop the infection and could decrease your chances of having complications later on. Medication for chlamydia should not be shared with anyone.
Repeat infection with chlamydia is common. You should be tested again about three months after you are treated, even if your sex partner(s) was treated.
I was treated for chlamydia. When can I have sex again?
You should not have sex again until you and your sex partner(s) have completed treatment. If your doctor prescribes a single dose of medication, you should wait seven days after taking the medicine before having sex. If your doctor prescribes a medicine for you to take for seven days, you should wait until you have taken all of the doses before having sex.
What happens if I don't get treated?
The initial damage that chlamydia causes often goes unnoticed. However, chlamydia can lead to serious health problems.
If you are a woman, untreated chlamydia can spread to your uterus and fallopian tubes (tubes that carry fertilized eggs from the ovaries to the uterus), causing pelvic inflammatory disease(http://www.cdc.gov/std/pid/stdfact-pid.htm) (PID). PID often has no symptoms, however some women may have abdominal and pelvic pain. Even if it doesn’t cause symptoms initially, PID can cause permanent damage to your reproductive system and lead to long-term pelvic pain, inability to get pregnant(http://www.cdc.gov/std/infertility), and potentially deadly ectopic pregnancy(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm) (pregnancy outside the uterus).
Men rarely have health problems linked to chlamydia. Infection sometimes spreads to the tube that carries sperm from the testicles, causing pain and fever. Rarely, chlamydia can prevent a man from being able to have children.
What is genital herpes?
Genital herpes(http://www.cdc.gov/std/herpes/default.htm) is an STD caused by two types of viruses. The viruses are called herpes simplex type 1 and herpes simplex type 2.
How common is genital herpes?
Genital herpes is common in the United States. In the United States, about one out of every six people aged 14 to 49 years have genital herpes.
How is genital herpes spread?
You can get herpes by having vaginal, anal, or oral sex with someone who has the disease.
Fluids found in a herpes sore carry the virus, and contact with those fluids can cause infection. You can also get herpes from an infected sex partner who does not have a visible sore or who may not know he or she is infected because the virus can be released through your skin and spread the infection to your sex partner(s).
How can I reduce my risk of getting herpes?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting herpes:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
Herpes symptoms can occur in both male and female genital areas that are covered by a latex condom. However, outbreaks can also occur in areas that are not covered by a condom so condoms may not fully protect you from getting herpes.
I'm pregnant. How could genital herpes affect my baby?
If you are pregnant and have genital herpes, it is even more important for you to go to prenatal care visits. You need to tell your doctor if you have ever had symptoms of, been exposed to, or been diagnosed with genital herpes. Sometimes genital herpes infection can lead to miscarriage. It can also make it more likely for you to deliver your baby too early. Herpes infection can be passed from you to your unborn child and cause a potentially deadly infection (neonatal herpes). It is important that you avoid getting herpes during pregnancy.
If you are pregnant and have genital herpes, you may be offered herpes medicine towards the end of your pregnancy to reduce the risk of having any symptoms and passing the disease to your baby. At the time of delivery your doctor should carefully examine you for symptoms. If you have herpes symptoms at delivery, a ‘C-section’ is usually performed.
How do I know if I have genital herpes?
Most people who have herpes have no, or very mild symptoms. You may not notice mild symptoms or you may mistake them for another skin condition, such as a pimple or ingrown hair. Because of this, most people who have herpes do not know it.
Genital herpes sores usually appear as one or more blisters on or around the genitals, rectum or mouth. The blisters break and leave painful sores that may take weeks to heal. These symptoms are sometimes called “having an outbreak.” The first time someone has an outbreak they may also have flu-like symptoms such as fever, body aches, or swollen glands.
Repeat outbreaks of genital herpes are common, especially during the first year after infection. Repeat outbreaks are usually shorter and less severe than the first outbreak. Although the infection can stay in the body for the rest of your life, the number of outbreaks tends to decrease over a period of years.
You should be examined by your doctor if you notice any of these symptoms or if your partner has an STD or symptoms of an STD, such as an unusual sore, a smelly discharge, burning when urinating, or, for women specifically, bleeding between periods.
How will my doctor know if I have herpes?
Often times, your healthcare provider can diagnose genital herpes by simply looking at your symptoms. Providers can also take a sample from the sore(s) and test it. Have an honest and open talk with your health care provider and ask whether you should be tested for herpes or other STDs. Blood testing for Herpes is not recommended as part of routine screening. Site swabbing for DNA is considered the "Gold Standard of Care" for Herpes.
Can herpes be cured?
There is no cure for herpes. However, there are medicines that can prevent or shorten outbreaks. One of these herpes medicines can be taken daily, and makes it less likely that you will pass the infection on to your sex partner(s).
What happens if I don't get treated?
Genital herpes can cause painful genital sores and can be severe in people with suppressed immune systems. If you touch your sores or the fluids from the sores, you may transfer herpes to another part of your body, such as your eyes. Do not touch the sores or fluids to avoid spreading herpes to another part of your body. If you touch the sores or fluids, immediately wash your hands thoroughly to help avoid spreading your infection.
Some people who get genital herpes have concerns about how it will impact their overall health, sex life, and relationships. It is best for you to talk to a health care provider about those concerns, but it also is important to recognize that while herpes is not curable, it can be managed. Since a genital herpes diagnosis may affect how you will feel about current or future sexual relationships, it is important to understand how to talk to sexual partners about STDs. You can find one resource here: GYT Campaign.
If you are pregnant, there can be problems for you and your unborn child. See “I’m pregnant. How could genital herpes affect my baby?(http://www.cdc.gov/std/herpes/stdfact-herpes.htm#a5)” above for information about this.
Can I still have sex if I have herpes?
If you have herpes, you should tell your sex partner(s) and let him or her know that you do and the risk involved. Using condoms may help lower this risk but it will not get rid of the risk completely. Having sores or other symptoms of herpes can increase your risk of spreading the disease. Even if you do not have any symptoms, you can still infect your sex partners.
What is the link between genital herpes and HIV?
Genital herpes can cause sores or breaks in the skin or lining of the mouth, vagina, and rectum. The genital sores caused by herpes can bleed easily. When the sores come into contact with the mouth, vagina, or rectum during sex, they increase the risk of giving or getting HIV if you or your partner has HIV.
What is syphilis?
Syphilis is an STD that can cause long-term complications if not treated correctly. Symptoms in adults are divided into stages. These stages are primary, secondary, latent, and late syphilis.
How is syphilis spread?
You can get syphilis by direct contact with a syphilis sore during vaginal, anal, or oral sex. Sores can be found on the penis, vagina, anus, in the rectum, or on the lips and in the mouth. Syphilis can also be spread from an infected mother to her unborn baby(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm).
What does syphilis look like?
Syphilis has been called ‘the great imitator’ because it has so many possible symptoms, many of which look like symptoms from other diseases. The painless syphilis sore that you would get after you are first infected can be confused for an ingrown hair, zipper cut, or other seemingly harmless bump. The non-itchy body rash that develops during the second stage of syphilis can show up on the palms of your hands and soles of your feet, all over your body, or in just a few places. You could also be infected with syphilis and have very mild symptoms or none at all.
 (http://www.cdc.gov/std/syphilis/images/chancre-penile.htm)
(http://www.cdc.gov/std/syphilis/images/chancre-penile.htm)
Example of a primary syphilis sore.
How can I reduce my risk of getting syphilis?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting syphilis:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex. Condoms prevent transmission of syphilis by preventing contact with a sore. Sometimes sores occur in areas not covered by a condom. Contact with these sores can still transmit syphilis.
Am I at risk for syphilis?
Any sexually active person can get syphilis through unprotected vaginal, anal, or oral sex. Have an honest and open talk with your health care provider and ask whether you should be tested for syphilis or other STDs. You should get tested regularly for syphilis if you are pregnant, are a man who has sex with men(https://www.cdc.gov/std/syphilis/stdfact-msm-syphilis.htm), have HIV infection, and/or have partner(s) who have tested positive for syphilis.
I’m pregnant. How does syphilis affect my baby?
If you are pregnant(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm) and have syphilis, you can give the infection to your unborn baby. Having syphilis can lead to a low birth weight baby. It can also make it more likely you will deliver your baby too early or stillborn (a baby born dead). To protect your baby, you should be tested for syphilis during your pregnancy and at delivery and receive immediate treatment if you test positive.
An infected baby may be born without signs or symptoms of disease. However, if not treated immediately, the baby may develop serious problems within a few weeks. Untreated babies can have health problems such as cataracts, deafness, or seizures, and can die.
 (http://www.cdc.gov/std/syphilis/images/rash-palmar.htm)
(http://www.cdc.gov/std/syphilis/images/rash-palmar.htm)
Secondary rash from syphilis on palms of hands.
How do I know if I have syphilis?
Symptoms of syphilis in adults can be divided into stages:
Primary Stage
During the first (primary) stage of syphilis, you may notice a single sore, but there may be multiple sores. The sore is the location where syphilis entered your body. The sore is usually firm, round, and painless. Because the sore is painless, it can easily go unnoticed. The sore lasts 3 to 6 weeks and heals regardless of whether or not you receive treatment. Even though the sore goes away, you must still receive treatment so your infection does not move to the secondary stage.
Secondary Stage
During the secondary stage, you may have skin rashes and/or sores in your mouth, vagina, or anus (also called mucous membrane lesions). This stage usually starts with a rash on one or more areas of your body. The rash can show up when your primary sore is healing or several weeks after the sore has healed. The rash can look like rough, red, or reddish brown spots on the palms of your hands and/or the bottoms of your feet. The rash usually won’t itch and it is sometimes so faint that you won’t notice it. Other symptoms you may have can include fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue (feeling very tired). The symptoms from this stage will go away whether or not you receive treatment. Without the right treatment, your infection will move to the latent and possibly late stages of syphilis.
 (http://www.cdc.gov/std/syphilis/images/rash-gbr.htm)
(http://www.cdc.gov/std/syphilis/images/rash-gbr.htm)
Secondary rash from syphilis on torso.
Latent and Late Stages
The latent stage of syphilis begins when all of the symptoms you had earlier disappear. If you do not receive treatment, you can continue to have syphilis in your body for years without any signs or symptoms. Most people with untreated syphilis do not develop late stage syphilis. However, when it does happen it is very serious and would occur 10–30 years after your infection began. Symptoms of the late stage of syphilis include difficulty coordinating your muscle movements, paralysis (not able to move certain parts of your body), numbness, blindness, and dementia (mental disorder). In the late stages of syphilis, the disease damages your internal organs and can result in death.
A syphilis infection is called an ‘early’ case(http://www.cdc.gov/std/stats10/app-casedef.htm#Syphilis) if a patient has been infected for a year or less, such as during the primary or secondary stages of syphilis. People who have ‘early’ syphilis infections can more easily spread the infection to their sex partners. The majority of early syphilis cases are currently found among men who have sex with men(http://www.cdc.gov/msmhealth/STD-syphilis-graph.htm), but women and unborn children are also at risk of infection.
How will my doctor know if I have syphilis?
Most of the time, a blood test can be used to test for syphilis. Some health care providers will diagnose syphilis by testing fluid from a syphilis sore.
Can syphilis be cured?
 (http://www.cdc.gov/std/syphilis/images/treponema-pallidum.htm)
(http://www.cdc.gov/std/syphilis/images/treponema-pallidum.htm)
Darkfield micrograph of Treponema pallidum.
Yes, syphilis can be cured with the right antibiotics from your health care provider. However, treatment will not undo any damage that the infection has already done.
I’ve been treated. Can I get syphilis again?
Having syphilis once does not protect you from getting it again. Even after you’ve been successfully treated, you can still be re-infected. Only laboratory tests can confirm whether you have syphilis. Follow-up testing by your health care provider is recommended to make sure that your treatment was successful.
Because syphilis sores can be hidden in the vagina, anus, under the foreskin of the penis, or in the mouth, it may not be obvious that a sex partner has syphilis. Unless you know that your sex partner(s) has been tested and treated, you may be at risk of getting syphilis again from an untreated sex partner.
What is Hepatitis A?
Hepatitis A is a contagious liver disease that results from infection with the Hepatitis A virus. It can range in severity from a mild illness lasting a few weeks to a severe illness lasting several months. Hepatitis A is usually spread when a person ingests fecal matter — even in microscopic amounts — from contact with objects, food, or drinks contaminated by the feces, or stool, of an infected person.
Statistics
How common is Hepatitis A in the United States?
In 2013, there were an estimated 3,473 acute hepatitis A infection in the United States.
Is Hepatitis A decreasing in the United States?
Yes. Rates of Hepatitis A in the United States are the lowest they have been in 40 years. The Hepatitis A vaccine was introduced in 1995 and health professionals now routinely vaccinate all children, travelers to certain countries, and persons at risk for the disease. Many experts believe Hepatitis A vaccination has dramatically affected rates of the disease in the United States.
Transmission / Exposure
How is Hepatitis A spread?
Hepatitis A is usually spread when the Hepatitis A virus is taken in by mouth from contact with objects, food, or drinks contaminated by the feces (or stool) of an infected person. A person can get Hepatitis A through:
- Person to person contact
- when an infected person does not wash his or her hands properly after going to the bathroom and touches other objects or food
- when a parent or caregiver does not properly wash his or her hands after changing diapers or cleaning up the stool of an infected person
- when someone has sex or sexual contact with an infected person. (not limited to anal-oral contact)
- Contaminated food or water
- Hepatitis A can be spread by eating or drinking food or water contaminated with the virus. (This can include frozen or undercooked food.) This is more likely to occur in countries where Hepatitis A is common and in areas where there are poor sanitary conditions or poor personal hygiene. The food and drinks most likely to be contaminated are fruits, vegetables, shellfish, ice, and water. In the United States, chlorination of water kills Hepatitis A virus that enters the water supply.
Who is at risk for Hepatitis A?
Although anyone can get Hepatitis A, in the United States, certain groups of people are at higher risk, such as those who:
- Travel to or live in countries where Hepatitis A is common
- Are men who have sexual contact with other men
- Use illegal drugs, whether injected or not
- Have clotting-factor disorders, such as hemophilia
- Live with someone who has Hepatitis A
- Have oral-anal sexual contact with someone who has Hepatitis A
I think I have been exposed to Hepatitis A. What should I do?
If you have any questions about potential exposure to Hepatitis A, call your health professional or your local or state health department.
If you were recently exposed to Hepatitis A virus and have not been vaccinated against Hepatitis A, you might benefit from an injection of either immune globulin(http://www.cdc.gov/hepatitis/hav/afaq.htm#vacIG) or Hepatitis A vaccine. However, the vaccine or immune globulin must be given within the first 2 weeks after exposure to be effective. A health professional can decide what is best on the basis of your age and overall health.
What should I do if I ate at a restaurant that had an outbreak of Hepatitis A?
Talk to your health professional or a local health department official for guidance. Outbreaks usually result from one of two sources of contamination: an infected food handler or an infected food source. Your health department will investigate the cause of the outbreak.
Keep in mind that most people do not get sick when someone at a restaurant has Hepatitis A. However, if an infected food handler is infectious and has poor hygiene, the risk goes up for patrons of that restaurant. In such cases, health officials might try to identify patrons and provide Hepatitis A vaccine or immune globulin(http://www.cdc.gov/hepatitis/hav/afaq.htm#vacIG) if they can find them within 2 weeks of exposure.
On rare occasions, the source of the infection can be traced to contaminated food. Foods can become contaminated at any point along the process: growing, harvesting, processing, handling, and even after cooking. In these cases, health officials will try to determine the source of the contamination and the best ways to minimize health threats to the public.
What is postexposure prophylaxis or PEP?
PEP or postexposure prophylaxis refers to trying to prevent or treat a disease after someone is exposed to it.
Who should get PEP after being exposed to Hepatitis A?
A health professional can decide whether or not a person needs PEP after exposure to Hepatitis A. People who might benefit from PEP include those who:
- Live with someone who has Hepatitis A
- Have recently had sexual contact with someone who has Hepatitis A
- Have recently shared injection or non-injection illegal drugs with someone who has Hepatitis A
- Have had ongoing, close personal contact with a person with Hepatitis A, such as a regular babysitter or caregiver
- Have been exposed to food or water known to be contaminated with Hepatitis A virus
If I have had Hepatitis A in the past, can I get it again?
No. Once you recover from Hepatitis A, you develop antibodies that protect you from the virus for life. An antibody is a substance found in the blood that the body produces in response to a virus. Antibodies protect the body from disease by attaching to the virus and destroying it.
Can I donate blood if I have had Hepatitis A?
If you had Hepatitis A when you were 11 years of age or older, you cannot donate blood. If you had Hepatitis A before age 11, you may be able donate blood. Check with your blood donation center.
How long does Hepatitis A virus survive outside the body?
The Hepatitis A virus is extremely hearty. It is able to survive the body’s highly acidic digestive tract and can live outside the body for months. High temperatures, such as boiling or cooking food or liquids for at least 1 minute at 185°F (85°C), kill the virus, although freezing temperatures do not.
Symptoms
Does Hepatitis A cause symptoms?
Not always. Some people get Hepatitis A and have no symptoms of the disease. Adults are more likely to have symptoms than children.
What are the symptoms of Hepatitis A?
Some people with Hepatitis A do not have any symptoms. If you do have symptoms, they may include the following:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (a yellowing of the skin or eyes)
How soon after exposure to Hepatitis A will symptoms appear?
If symptoms occur, they usually appear anywhere from 2 to 6 weeks after exposure. Symptoms usually develop over a period of several days.
How long do Hepatitis A symptoms last?
Symptoms usually last less than 2 months, although some people can be ill for as long as 6 months.
Can a person spread Hepatitis A without having symptoms?
Yes. Many people, especially children, have no symptoms. In addition, a person can transmit the virus to others up to 2 weeks before symptoms appear.
How serious is Hepatitis A?
Almost all people who get Hepatitis A recover completely and do not have any lasting liver damage, although they may feel sick for months. Hepatitis A can sometimes cause liver failure and death, although this is rare and occurs more commonly in persons 50 years of age or older and persons with other liver diseases, such as Hepatitis B or C.
Diagnosis / Treatment
How will I know if I have Hepatitis A?
A doctor can determine if you have Hepatitis A by discussing your symptoms and taking a blood sample.
How is Hepatitis A treated?
There are no special treatments for Hepatitis A. Most people with Hepatitis A will feel sick for a few months before they begin to feel better. A few people will need to be hospitalized. During this time, doctors usually recommend rest, adequate nutrition, and fluids. People with Hepatitis A should check with a health professional before taking any prescription pills, supplements, or over-the-counter medications, which can potentially damage the liver. Alcohol should be avoided.
Prevention / Vaccination
Can Hepatitis A be prevented?
Yes. The best way to prevent Hepatitis A is through vaccination with the Hepatitis A vaccine. Vaccination is recommended for all children, for travelers to certain countries, and for people at high risk for infection with the virus. Frequent handwashing with soap and warm water after using the bathroom, changing a diaper, or before preparing food can help prevent the spread of Hepatitis A.
What is the Hepatitis A vaccine?
The Hepatitis A vaccine is a shot of inactive Hepatitis A virus that stimulates the body's natural immune system. After the vaccine is given, the body makes antibodies that protect a person against the virus. An antibody is a substance found in the blood that is produced in response to a virus invading the body. These antibodies are then stored in the body and will fight off the infection if a person is exposed to the virus in the future.
Who should get vaccinated against Hepatitis A?
Hepatitis A vaccination is recommended for:
- All children at age 1 year
- Travelers to countries that have high rates of Hepatitis A
- Men who have sexual contact with other men
- Users of injection and non-injection illegal drugs
- People with chronic (lifelong) liver diseases, such as Hepatitis B or Hepatitis C
- People who are treated with clotting-factor concentrates
- People who work with Hepatitis A infected animals or in a Hepatitis A research laboratory
How is the Hepatitis A vaccine given?
The Hepatitis A vaccine is given as 2 shots, 6 months apart. The Hepatitis A vaccine also comes in a combination form, containing both Hepatitis A and B vaccine, that can be given to persons 18 years of age and older. This form is given as 3 shots, over a period of 6 months.
Is the Hepatitis A vaccine effective?
Yes, the Hepatitis A vaccine is highly effective in preventing Hepatitis A virus infection. Protection begins approximately 2 to 4 weeks after the first injection. A second injection results in long-term protection.
Is the Hepatitis A vaccine safe?
Yes, the Hepatitis A vaccine is safe. No serious side effects have resulted from the Hepatitis A vaccine. Soreness at the injection site is the most common side effect reported. As with any medicine, there are very small risks that a serious problem could occur after someone gets the vaccine. However, the potential risks associated with Hepatitis A are much greater than the potential risks associated with the Hepatitis A vaccine. Before the Hepatitis A vaccine became available in the Unites States, more than 250,000 people were infected with Hepatitis A virus each year. Since the licensure of the first Hepatitis A vaccine in 1995, millions of doses of Hepatitis A vaccine have been given in the United States and worldwide.
Who should not receive the Hepatitis A vaccine?
People who have ever had a serious allergic reaction to the Hepatitis A vaccine or who are known to be allergic to any part of the Hepatitis A vaccine should not receive the vaccine. Tell your doctor if you have any severe allergies. Also, the vaccine is not licensed for use in infants under age 1 year.
Who should get the Hepatitis A vaccine before traveling?
Anyone traveling to or working in countries with high rates of Hepatitis A should talk to a health professional about getting vaccinated. He or she is likely to recommend vaccination or a shot of immune globulin before traveling to countries in Central or South America, Mexico, and certain parts of Asia, Africa, and Eastern Europe. CDC’s Travelers’ Health site provides detailed information about Hepatitis A and other recommended vaccines at wwwn.cdc.gov/travel/yellowBookCH4-HepA.aspx.
What is immune globulin?
Immune globulin is a substance made from human blood plasma that contains antibodies that protect against infection. It is given as a shot and provides short-term protection (approximately 3 months) against Hepatitis A. Immune globulin can be given either before exposure to the Hepatitis A virus (such as before travel to a country where Hepatitis A is common) or to prevent infection after exposure to the Hepatitis A virus. Immune globulin must be given within 2 weeks after exposure for the best protection.
Why is the Hepatitis A vaccine recommended before traveling?
Traveling to places where Hepatitis A virus is common puts a person at high risk for Hepatitis A. The risk exists even for travelers to urban areas, those who stay in luxury hotels, and those who report that they have good hygiene and are careful about what they eat and drink. Travelers can minimize their risk by avoiding potentially contaminated water or food, such as drinking beverages (with or without ice) of unknown purity, eating uncooked shellfish, and eating uncooked fruits or vegetables that are not peeled or prepared by the traveler personally. Risk for infection increases with duration of travel and is highest for those who live in or visit rural areas, trek in back-country areas, or frequently eat or drink in settings with poor sanitation. Since a simple, safe vaccine exists, experts recommend that travelers to certain countries be vaccinated.
How soon before travel should the Hepatitis A vaccine be given?
The first dose of Hepatitis A vaccine should be given as soon as travel is planned. Two weeks or more before departure is ideal, but anytime before travel will provide some protection.
I'm leaving for my trip in a few days. Can I still get the Hepatitis A vaccine?
Experts now say that the first dose of Hepatitis A vaccine can be given at any time before departure. This will provide some protection for most healthy persons.
Will the Hepatitis A vaccine protect someone from other forms of hepatitis?
Hepatitis A vaccine will only protect someone from Hepatitis A. A separate vaccine is available for Hepatitis B. There is also a combination vaccine that protects a person from Hepatitis A and Hepatitis B. No vaccine is available for Hepatitis C at this time.
Can Hepatitis A vaccine be given to immunocompromised persons, such as hemodialysis patients or persons with AIDS?
Yes. Because Hepatitis A vaccine is inactivated (not “live”), it can be given to people with compromised immune systems.
Is it harmful to have an extra dose of Hepatitis A vaccine or to repeat the entire Hepatitis A vaccine series?
No, getting extra doses of Hepatitis A vaccine is not harmful.
What should be done if the last dose of Hepatitis A vaccine is delayed?
The second or last dose should be given by a health professional as soon as possible. The first dose does not need to be given again
What is hepatitis B?
Hepatitis B is a serious infection that affects the liver. It is caused by the hepatitis B virus.
- In 2009, about 38,000 people became infected with hepatitis B.
- Each year about 2,000 to 4,000 people die in the United States from cirrhosis or liver cancer caused by hepatitis B.
Hepatitis B can cause:
Acute (short-term) illness. This can lead to:
- loss of appetite
- tiredness
- pain in muscles, joints, and stomach
- diarrhea and vomiting
- jaundice (yellow skin or eyes)
Acute illness, with symptoms, is more common among adults. Children who become infected usually do not have symptoms.
Chronic (long-term) infection. Some people go on to develop chronic hepatitis B infection. Most of them do not have symptoms, but the infection is still very serious, and can lead to:
- liver damage (cirrhosis)
- liver cancer
- death
Chronic infection is more common among infants and children than among adults. People who are chronically infected can spread hepatitis B virus to others, even if they don’t look or feel sick. Up to 1.4 million people in the United States may have chronic hepatitis B infection.
Hepatitis B virus is easily spread through contact with the blood or other body fluids of an infected person. People can also be infected from contact with a contaminated object, where the virus can live for up to 7 days.
- A baby whose mother is infected can be infected at birth;
- Children, adolescents, and adults can become infected by:
- contact with blood and body fluids through breaks in the skin such as bites, cuts, or sores;
- contact with objects that have blood or body fluids on them such as toothbrushes, razors, or monitoring and treatment devices for diabetes;
- having unprotected sex with an infected person;
- sharing needles when injecting drugs;
- being stuck with a used needle.
Hepatitis B vaccine: Why get vaccinated?
Hepatitis B vaccine can prevent hepatitis B, and the serious consequences of hepatitis B infection, including liver cancer and cirrhosis.
Hepatitis B vaccine may be given by itself or in the same shot with other vaccines.
Routine hepatitis B vaccination was recommended for some U.S. adults and children beginning in 1982, and for all children in 1991. Since 1990, new hepatitis B infections among children and adolescents have dropped by more than 95% – and by 75% in other age groups.
Vaccination gives long-term protection from hepatitis B infection, possibly lifelong.
Who should get hepatitis B vaccine and when?
Children and adolescents
- Babies normally get 3 doses of hepatitis B vaccine:
- 1st Dose: Birth
- 2nd Dose: 1-2 months of age
- 3rd Dose: 6-18 months of age
Some babies might get 4 doses, for example, if a combination vaccine containing hepatitis B is used. (This is a single shot containing several vaccines.) The extra dose is not harmful.
- Anyone through 18 years of age who didn't get the vaccine when they were younger should also be vaccinated.
Adults
- All unvaccinated adults at risk for hepatitis B infection should be vaccinated. This includes:
- sex partners of people infected with hepatitis B,
- men who have sex with men,
- people who inject street drugs,
- people with more than one sex partner,
- people with chronic liver or kidney disease,
- people under 60 years of age with diabetes,
- people with jobs that expose them to human blood or other body fluids,
- household contacts of people infected with hepatitis B,
- residents and staff in institutions for the developmentally disabled,
- kidney dialysis patients,
- people who travel to countries where hepatitis B is common,
- people with HIV infection.
- Other people may be encouraged by their doctor to get hepatitis B vaccine; for example, adults 60 and older with diabetes. Anyone else who wants to be protected from hepatitis B infection may get the vaccine.
- Pregnant women who are at risk for one of the reasons stated above should be vaccinated. Other pregnant women who want protection may be vaccinated.
Adults getting hepatitis B vaccine should get 3 doses — with the second dose given 4 weeks after the first and the third dose 5 months after the second. Your doctor can tell you about other dosing schedules that might be used in certain circumstances.
Who should not get hepatitis B vaccine?
- Anyone with a life-threatening allergy to yeast, or to any other component of the vaccine, should not get hepatitis B vaccine. Tell your doctor if you have any severe allergies.
- Anyone who has had a life-threatening allergic reaction to a previous dose of hepatitis B vaccine should not get another dose.
- Anyone who is moderately or severely ill when a dose of vaccine is scheduled should probably wait until they recover before getting the vaccine.
Your doctor can give you more information about these precautions.
Note: You might be asked to wait 28 days before donating blood after getting hepatitis B vaccine. This is because the screening test could mistake vaccine in the bloodstream (which is not infectious) for hepatitis B infection.
What are the risks from hepatitis B vaccine?
Hepatitis B is a very safe vaccine. Most people do not have any problems with it.
The vaccine contains non-infectious material, and cannot cause hepatitis B infection.
Some mild problems have been reported:
- Soreness where the shot was given (up to about 1 person in 4).
- Temperature of 99.9°F or higher (up to about 1 person in 15).
Severe problems are extremely rare. Severe allergic reactions are believed to occur about once in 1.1 million doses.
A vaccine, like any medicine, could cause a serious reaction. But the risk of a vaccine causing serious harm, or death, is extremely small. More than 100 million people in the United States have been vaccinated with hepatitis B vaccine.
What if there is a serious reaction?
What should I look for?
-
Look for anything that concerns you, such as signs of a severe allergic reaction, very high fever, or behavior changes.
Signs of a severe allergic reaction can include hives, swelling of the face and throat, difficulty breathing, a fast heartbeat, dizziness, and weakness. These would start a few minutes to a few hours after the vaccination.
What should I do?
- If you think it is a severe allergic reaction or other emergency that can’t wait, call 9-1-1 or get the person to the nearest hospital. Otherwise, call your doctor.
- Afterward, the reaction should be reported to the Vaccine Adverse Event Reporting System (VAERS). Your doctor might file this report, or you can do it yourself through the VAERS website, or by calling 1-800-822-7967.
VAERS is only for reporting reactions. They do not give medical advice.
What is Hepatitis C?
Hepatitis C is a contagious liver disease that ranges in severity from a mild illness lasting a few weeks to a serious, lifelong illness that attacks the liver. It results from infection with the Hepatitis C virus (HCV), which is spread primarily through contact with the blood of an infected person. Hepatitis C can be either “acute” or “chronic.”
Acute Hepatitis C virus infection is a short-term illness that occurs within the first 6 months after someone is exposed to the Hepatitis C virus. For most people, acute infection leads to chronic infection.
Chronic Hepatitis C virus infection is a long-term illness that occurs when the Hepatitis C virus remains in a person’s body. Hepatitis C virus infection can last a lifetime and lead to serious liver problems, including cirrhosis (scarring of the liver) or liver cancer.
Statistics
How common is acute Hepatitis C in the United States?
In 2013, there were an estimated 29,718 cases of acute hepatitis C virus infections reported in the United States.
How common is chronic Hepatitis C in the United States?
An estimated 2.7 million persons in the United States have chronic hepatitis C virus infection. Most people do not know they are infected because they don’t look or feel sick.
How likely is it that acute Hepatitis C will become chronic?
Approximately 75%–85% of people who become infected with Hepatitis C virus develop chronic infection.
Transmission / Exposure
How is Hepatitis C spread?
Hepatitis C is usually spread when blood from a person infected with the Hepatitis C virus enters the body of someone who is not infected. Today, most people become infected with the Hepatitis C virus by sharing needles or other equipment to inject drugs. Before 1992, when widespread screening of the blood supply began in the United States, Hepatitis C was also commonly spread through blood transfusions and organ transplants.
People can become infected with the Hepatitis C virus during such activities as
- Sharing needles, syringes, or other equipment to inject drugs
- Needlestick injuries in health care settings
- Being born to a mother who has Hepatitis C
Less commonly, a person can also get Hepatitis C virus infection through
- Sharing personal care items that may have come in contact with another person’s blood, such as razors or toothbrushes
- Having sexual contact with a person infected with the Hepatitis C virus
Can Hepatitis C be spread through sexual contact?
Yes, but the risk of transmission from sexual contact is believed to be low. The risk increases for those who have multiple sex partners, have a sexually transmitted disease, engage in rough sex, or are infected with HIV. More research is needed to better understand how and when Hepatitis C can be spread through sexual contact.
Can you get Hepatitis C by getting a tattoo or piercing?
A few major research studies have not shown Hepatitis C to be spread through licensed, commercial tattooing facilities. However, transmission of Hepatitis C (and other infectious diseases) is possible when poor infection-control practices are used during tattooing or piercing. Body art is becoming increasingly popular in the United States, and unregulated tattooing and piercing are known to occur in prisons and other informal or unregulated settings. Further research is needed to determine if these types of settings and exposures are responsible for Hepatitis C virus transmission.
Can Hepatitis C be spread within a household?
Yes, but this does not occur very often. If Hepatitis C virus is spread within a household, it is most likely a result of direct, through-the-skin exposure to the blood of an infected household member.
How should blood spills be cleaned from surfaces to make sure that Hepatitis C virus is gone?
Any blood spills — including dried blood, which can still be infectious — should be cleaned using a dilution of one part household bleach to 10 parts water. Gloves should be worn when cleaning up blood spills.
How long does the Hepatitis C virus survive outside the body?
The Hepatitis C virus can survive outside the body at room temperature, on environmental surfaces, for up to 3 weeks.
What are ways Hepatitis C is not spread?
Hepatitis C virus is not spread by sharing eating utensils, breastfeeding, hugging, kissing, holding hands, coughing, or sneezing. It is also not spread through food or water.
Who is at risk for Hepatitis C?
Some people are at increased risk for Hepatitis C, including
- Current injection drug users (currently the most common way Hepatitis C virus is spread in the United States)
- Past injection drug users, including those who injected only one time or many years ago
- Recipients of donated blood, blood products, and organs (once a common means of transmission but now rare in the United States since blood screening became available in 1992)
- People who received a blood product for clotting problems made before 1987
- Hemodialysis patients or persons who spent many years on dialysis for kidney failure
- People who received body piercing or tattoos done with non-sterile instruments
- People with known exposures to the Hepatitis C virus, such as
- Health care workers injured by needlesticks
- Recipients of blood or organs from a donor who tested positive for the Hepatitis C virus
- HIV-infected persons
- Children born to mothers infected with the Hepatitis C virus
Less common risks include:
- Having sexual contact with a person who is infected with the Hepatitis C virus
- Sharing personal care items, such as razors or toothbrushes, that may have come in contact with the blood of an infected person
What is the risk of a pregnant woman passing Hepatitis C to her baby?
Hepatitis C is rarely passed from a pregnant woman to her baby. About 6 of every 100 infants born to mothers with Hepatitis C become infected with the virus. However, the risk becomes greater if the mother has both HIV infection and Hepatitis C.
Can a person get Hepatitis C from a mosquito or other insect bite?
Hepatitis C virus has not been shown to be transmitted by mosquitoes or other insects.
Can I donate blood, organs, or semen if I have Hepatitis C?
No, if you ever tested positive for the Hepatitis C virus (or Hepatitis B virus), experts recommend never donating blood, organs, or semen because this can spread the infection to the recipient.
Symptoms
What are the symptoms of acute Hepatitis C?
Approximately 70%–80% of people with acute Hepatitis C do not have any symptoms. Some people, however, can have mild to severe symptoms soon after being infected, including
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (yellow color in the skin or eyes)
How soon after exposure to Hepatitis C do symptoms appear?
If symptoms occur, the average time is 6–7 weeks after exposure, but this can range from 2 weeks to 6 months. However, many people infected with the Hepatitis C virus do not develop symptoms.
Can a person spread Hepatitis C without having symptoms?
Yes, even if a person with Hepatitis C has no symptoms, he or she can still spread the virus to others.
Is it possible to have Hepatitis C and not know it?
Yes, many people who are infected with the Hepatitis C virus do not know they are infected because they do not look or feel sick.
What are the symptoms of chronic Hepatitis C?
Most people with chronic Hepatitis C do not have any symptoms. However, if a person has been infected for many years, his or her liver may be damaged. In many cases, there are no symptoms of the disease until liver problems have developed. In persons without symptoms, Hepatitis C is often detected during routine blood tests to measure liver function and liver enzyme (protein produced by the liver) level.
How serious is chronic Hepatitis C?
Chronic Hepatitis C is a serious disease that can result in long-term health problems, including liver damage, liver failure, liver cancer, or even death. It is the leading cause of cirrhosis and liver cancer and the most common reason for liver transplantation in the United States. Approximately 15,000 people die every year from Hepatitis C related liver disease.
What are the long-term effects of Hepatitis C?
Of every 100 people infected with the Hepatitis C virus, about
- 75–85 people will develop chronic Hepatitis C virus infection; of those,
- 60–70 people will go on to develop chronic liver disease
- 5–20 people will go on to develop cirrhosis over a period of 20–30 years
- 1–5 people will die from cirrhosis or liver cancer
Tests
Can a person have normal liver enzyme (e.g., ALT) results and still have Hepatitis C?
Yes. It is common for persons with chronic Hepatitis C to have a liver enzyme level that goes up and down, with periodic returns to normal or near normal. Some infected persons have liver enzyme levels that are normal for over a year even though they have chronic liver disease. If the liver enzyme level is normal, persons should have their enzyme level re-checked several times over a 6–12 month period. If the liver enzyme level remains normal, the doctor may check it less frequently, such as once a year.
Who should get tested for Hepatitis C?
Talk to your doctor about being tested for Hepatitis C if any of the following are true:
- You were born from 1945 through 1965
- You are a current or former injection drug user, even if you injected only one time or many years ago.
- You were treated for a blood clotting problem before 1987.
- You received a blood transfusion or organ transplant before July 1992.
- You are on long-term hemodialysis treatment.
- You have abnormal liver tests or liver disease.
- You work in health care or public safety and were exposed to blood through a needlestick or other sharp object injury.
- You are infected with HIV.
If you are pregnant, should you be tested for Hepatitis C?
No, getting tested for Hepatitis C is not part of routine prenatal care. However, if a pregnant woman has risk factors(http://www.cdc.gov/hepatitis/hcv/cfaq.htm) for Hepatitis C virus infection, she should speak with her doctor about getting tested.
What blood tests are used to test for Hepatitis C?
Several different blood tests are used to test for Hepatitis C. A doctor may order just one or a combination of these tests. Typically, a person will first get a screening test that will show whether he or she has developed antibodies to the Hepatitis C virus. (An antibody is a substance found in the blood that the body produces in response to a virus.) Having a positive antibody test means that a person was exposed to the virus at some time in his or her life. If the antibody test is positive, a doctor will most likely order a second test to confirm whether the virus is still present in the person's bloodstream.
Treatment
Can acute Hepatitis C be treated?
Yes, acute hepatitis C can be treated. Acute infection can clear on its own without treatment in about 25% of people. If acute hepatitis C is diagnosed, treatment does reduce the risk that acute hepatitis C will become a chronic infection. Acute hepatitis C is treated with the same medications used to treat chronic Hepatitis C. However, the optimal treatment and when it should be started remains uncertain.
Can chronic Hepatitis C be treated?
Yes. There are several medications available to treat chronic Hepatitis C, including new treatments that appear to be more effective and have fewer side effects than previous options. The Food and Drug Administration (FDA) maintains a complete list of approved treatments for Hepatitis C.
Is it possible to get over Hepatitis C?
Yes, approximately 15%–25% of people who get Hepatitis C will clear the virus from their bodies without treatment and will not develop chronic infection. Experts do not fully understand why this happens for some people.
What can a person with chronic Hepatitis C do to take care of his or her liver?
People with chronic Hepatitis C should be monitored regularly by an experienced doctor. They should avoid alcohol because it can cause additional liver damage. They also should check with a health professional before taking any prescription pills, supplements, or over-the-counter medications, as these can potentially damage the liver. If liver damage is present, a person should check with his or her doctor about getting vaccinated against Hepatitis A and Hepatitis B.
Vaccination
Is there a vaccine that can prevent Hepatitis C?
Not yet. Vaccines are available only for Hepatitis A and Hepatitis B. Research into the development of a vaccine is under way.
Hepatitis C and Employment
Should a person infected with the Hepatitis C virus be restricted from working in certain jobs or settings?
CDC's recommendations(http://www.cdc.gov/mmwr/preview/mmwrhtml/00055154.htm) for prevention and control of the Hepatitis C virus infection state that people should not be excluded from work, school, play, child care, or other settings because they have Hepatitis C. There is no evidence that people can get Hepatitis C from food handlers, teachers, or other service providers without blood-to-blood contact.
Hepatitis C and Co-infection with HIV
What is HIV and Hepatitis C virus coinfection?
HIV and Hepatitis C virus coinfection refers to being infected with both HIV and the Hepatitis C virus. Coinfection is more common in persons who inject drugs. In fact, 50%–90% of HIV-infected persons who use injection drugs are also infected with the Hepatitis C virus. To learn more about coinfection, visit http://www.cdc.gov/hiv/resources/factsheets/hepatitis.htm(http://www.cdc.gov/hiv/resources/factsheets/hepatitis.htm).
What is HPV?
HPV is the most common sexually transmitted infection (STI). HPV is a different virus than HIV(http://www.cdc.gov/hiv/basics) and HSV(http://www.cdc.gov/std/herpes/stdfact-herpes.htm) (herpes). HPV is so common that nearly all sexually active men and women get it at some point in their lives. There are many different types of HPV. Some types can cause health problems including genital warts and cancers. But there are vaccines that can stop these health problems from happening.
How is HPV spread?
You can get HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. HPV can be passed even when an infected person has no signs or symptoms.
Anyone who is sexually active can get HPV, even if you have had sex with only one person. You also can develop symptoms years after you have sex with someone who is infected making it hard to know when you first became infected.
Does HPV cause health problems?
In most cases, HPV goes away on its own and does not cause any health problems. But when HPV does not go away, it can cause health problems like genital warts and cancer.
Genital warts usually appear as a small bump or group of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. A healthcare provider can usually diagnose warts by looking at the genital area.
Does HPV cause cancer?
HPV can cause cervical and other cancers(http://www.cdc.gov/cancer/hpv) including cancer of the vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat, including the base of the tongue and tonsils (called oropharyngeal cancer(http://www.cdc.gov/cancer/hpv/statistics/headneck.htm)).
Cancer often takes years, even decades, to develop after a person gets HPV. The types of HPV that can cause genital warts are not the same as the types of HPV that can cause cancers.
There is no way to know which people who have HPV will develop cancer or other health problems. People with weak immune systems (including individuals with HIV/AIDS) may be less able to fight off HPV and more likely to develop health problems from it.
How can I avoid HPV and the health problems it can cause?
You can do several things to lower your chances of getting HPV.
Get vaccinated. HPV vaccines are safe and effective. They can protect males and females against diseases (including cancers) caused by HPV when given in the recommended age groups (see “Who should get vaccinated?” below). HPV vaccines are given in three shots over six months; it is important to get all three doses.
Get screened for cervical cancer. Routine screening for women aged 21 to 65 years old can prevent cervical cancer.
If you are sexually active
- Use latex condoms the right way every time you have sex. This can lower your chances of getting HPV. But HPV can infect areas that are not covered by a condom - so condoms may not give full protection against getting HPV;
- Be in a mutually monogamous relationship – or have sex only with someone who only has sex with you.
Who should get vaccinated?
All boys and girls ages 11 or 12 years should get vaccinated.
Catch-up vaccines are recommended for males through age 21 and for females through age 26, if they did not get vaccinated when they were younger.
The vaccine is also recommended for gay and bisexual men (or any man who has sex with a man) through age 26. It is also recommended for men and women with compromised immune systems (including people living with HIV/AIDS) through age 26, if they did not get fully vaccinated when they were younger.
How do I know if I have HPV?
There is no test to find out a person’s “HPV status.” Also, there is no approved HPV test to find HPV in the mouth or throat.
There are HPV tests that can be used to screen for cervical cancer. These tests are recommended for screening only in women aged 30 years and older. They are not recommended to screen men, adolescents, or women under the age of 30 years.
Most people with HPV do not know they are infected and never develop symptoms or health problems from it. Some people find out they have HPV when they get genital warts. Women may find out they have HPV when they get an abnormal Pap test result (during cervical cancer screening). Others may only find out once they’ve developed more serious problems from HPV, such as cancers.
How common is HPV and the health problems caused by HPV?
HPV (the virus): About 79 million Americans are currently infected with HPV. About 14 million people become newly infected each year. HPV is so common that most sexually-active men and women will get at least one type of HPV at some point in their lives.
Health problems related to HPV include genital warts and cervical cancer.
Genital warts: About 360,000 people in the United States get genital warts each year.
Cervical cancer: More than 11,000 women in the United States get cervical cancer each year.
There are other conditions and cancers(http://www.cdc.gov/std/hpv/stdfact-hpv.htm#a4) caused by HPV that occur in persons living in the United States.
I'm pregnant. Will having HPV affect my pregnancy?
If you are pregnant and have HPV, you can get genital warts or develop abnormal cell changes on your cervix. Abnormal cell changes can be found with routine cervical cancer screening. You should get routine cervical cancer screening even when you are pregnant.
Can I be treated for HPV or health problems caused by HPV?
There is no treatment for the virus itself. However, there are treatments for the health problems that HPV can cause:
- Genital warts can be treated by you or your physician. If left untreated, genital warts may go away, stay the same, or grow in size or number.
- Cervical precancer can be treated. Women who get routine Pap tests and follow up as needed can identify problems before cancer develops. Prevention is always better than treatment. For more information visit www.cancer.org.
- Other HPV-related cancers are also more treatable when diagnosed and treated early. For more information visit www.cancer.org.
Urethritis
Urethritis, as characterized by urethral inflammation, can result from infectious and noninfectious conditions. Symptoms, if present, include dysuria; urethral pruritis; and mucoid, mucopurulent, or purulent discharge. Signs of urethral discharge on examination can also be present in persons without symptoms. Although N. gonorrhoeae and C. trachomatis are well established as clinically important infectious causes of urethritis, Mycoplasma genitalium has also been associated with urethritis and, less commonly, prostatitis (470-474(http://www.cdc.gov/std/tg2015/references.htm#470)). If point-of-care diagnostic tools (e.g., Gram, methylene blue [MB] or gentian violet [GV] stain microscopy, first void urine with microscopy, and leukocyte esterase) are not available, drug regimens effective against both gonorrhea and chlamydia should be administered. Further testing to determine the specific etiology is recommended to prevent complications, re-infection, and transmission because a specific diagnosis might improve treatment compliance, delivery of risk reduction interventions, and partner notification. Both chlamydia and gonorrhea are reportable to health departments. NAATs are preferred for the detection of C. trachomatis and N. gonorrhoeae, and urine is the preferred specimen in males (394(http://www.cdc.gov/std/tg2015/references.htm#394)). NAAT-based tests for the diagnosis of T. vaginalis in men have not been cleared by FDA; however, some laboratories have performed the CLIA-compliant validation studies (475(http://www.cdc.gov/std/tg2015/references.htm#475)) needed to provide such testing.
Etiology
Several organisms can cause infectious urethritis. The presence of Gram-negative intracellular diplococci (GNID) or MB/GV purple intracellular diplococci on urethral smear is indicative of presumed gonorrhea infection, which is frequently accompanied by chlamydial infection. NGU, which is diagnosed when microscopy of urethral secretions indicates inflammation without GNID or MB/GV purple intracellular diplococci, is caused by C. trachomatis in 15%–40% of cases; however, prevalence varies by age group, with a lower burden of disease occurring among older men (476(http://www.cdc.gov/std/tg2015/references.htm#476)). Documentation of chlamydial infection as the etiology of NGU is essential because of the need for partner referral for evaluation and treatment to prevent complications of chlamydia, especially in female partners. Complications of C. trachomatis-associated NGU among males include epididymitis, prostatitis, and reactive arthritis.
M. genitalium, which can be sexually transmitted, is associated with symptoms of urethritis as well as urethral inflammation and accounts for 15%–25% of NGU cases in the United States (470-473(http://www.cdc.gov/std/tg2015/references.htm#470)). However, FDA-cleared diagnostic tests for M. genitalium are not available.
T. vaginalis can cause NGU in heterosexual men, but the prevalence varies substantially by region of the United States and within specific subpopulations. In some instances, NGU can be acquired by fellatio (i.e., oral penile contact), sometimes because of specific pathogens such as HSV, Epstein Barr Virus, and adenovirus (476(http://www.cdc.gov/std/tg2015/references.htm#476)); data supporting other Mycoplasma species and Ureaplasma as etiologic agents are inconsistent. Diagnostic and treatment procedures for these organisms are reserved for situations in which these infections are suspected (e.g., contact with trichomoniasis, urethral lesions, or severe dysuria and meatitis, which might suggest genital herpes) or when NGU is not responsive to recommended therapy. Enteric bacteria have been identified as an uncommon cause of NGU and might be associated with insertive anal intercourse (476(http://www.cdc.gov/std/tg2015/references.htm#476)). The importance of NGU not caused by defined pathogens is uncertain; neither complications (e.g., urethral stricture and epididymitis) nor adverse outcomes in sex partners have been identified in these cases.
Diagnostic Considerations
Clinicians should attempt to obtain objective evidence of urethral inflammation. However, if point-of-care diagnostic tests (e.g., Gram, MB or GV, or Gram stain microscopy) are not available, all men should be tested by NAAT and treated with drug regimens effective against both gonorrhea and chlamydia.
In the setting of compatible symptoms, urethritis can be documented on the basis of any of the following signs or laboratory tests:
- Mucoid, mucopurulent, or purulent discharge on examination.
- Gram stain of urethral secretions demonstrating ≥2 WBC per oil immersion field (477(http://www.cdc.gov/std/tg2015/references.htm#477)). The Gram stain is a point-of-care diagnostic test for evaluating urethritis that is highly sensitive and specific for documenting both urethritis and the presence or absence of gonococcal infection. MB/GV stain of urethral secretions is an alternative point-of-care diagnostic test with performance characteristics similar to Gram stain; thus, the cutoff number for WBC per oil immersion field should be the same (478(http://www.cdc.gov/std/tg2015/references.htm#478)). Presumed gonococcal infection is established by documenting the presence of WBC containing GNID in Gram stain or intracellular purple diplococci in MB/GV smears; men should be presumptively treated and managed accordingly for gonorrhea (GC) infection (see Gonococcal Infections(http://www.cdc.gov/std/tg2015/gonorrhea.htm)).
- Positive leukocyte esterase test on first-void urine or microscopic examination of sediment from a spun first-void urine demonstrating ≥10 WBC per high power field.
In settings where Gram stain or MB/GV smear is available, men who meet criteria for urethritis (microscopy of urethral secretions with >2 WBC per oil immersion field and no intracellular gram negative or purple diplococci) should receive NAAT testing for C. trachomatis and N. gonorrhoeae and can be managed as recommended (see Nongonococcal Urethritis(http://www.cdc.gov/std/tg2015/urethritis-and-cervicitis.htm#nongon)). Men evaluated in settings in which Gram stain or MB/GV smear is not available (i.e., gonococcal infection cannot be ruled out at the point of care) who meet at least one criterion for urethritis (i.e., urethral discharge, positive LE test on first void urine, or microscopic exam of first void urine sediment with > 10 WBC per hpf) should be tested by NAAT and treated with regimens effective against gonorrhea and chlamydia.
If symptoms are present but no evidence of urethral inflammation is present, NAAT testing for C. trachomatis and N. gonorrhoeae might identify infections (479(http://www.cdc.gov/std/tg2015/references.htm#479)). If the results demonstrate infection with these pathogens, the appropriate treatment should be given and sex partners referred for evaluation and treatment. If none of these clinical criteria are present, empiric treatment of symptomatic men is recommended only for those men at high risk for infection who are unlikely to return for a follow-up evaluation or test results. Such men should be treated with drug regimens effective against gonorrhea and chlamydia.
Nongonococcal Urethritis
Diagnostic Considerations
NGU is a nonspecific diagnosis that can have many infectious etiologies. NGU is confirmed in symptomatic men when staining of urethral secretions indicates inflammation without Gram negative or purple diplococci. All men who have confirmed NGU should be tested for chlamydia and gonorrhea even if point-of-care tests are negative for evidence of GC. NAATs for chlamydia and gonorrhea are recommended because of their high sensitivity and specificity; a specific diagnosis can potentially reduce complications, re-infection, and transmission (394(http://www.cdc.gov/std/tg2015/references.htm#394)). Testing for T. vaginalis should be considered in areas or populations of high prevalence.
Treatment
Presumptive treatment should be initiated at the time of NGU diagnosis. Azithromycin and doxycycline are highly effective for chlamydial urethritis. NGU associated with M. genitalium currently responds better to azithromycin than doxycycline, although azithromycin efficacy might be declining (See Mycoplasma genitalium(http://www.cdc.gov/std/tg2015/emerging.htm#myco)).
Other Management Considerations
To minimize transmission and reinfection, men treated for NGU should be instructed to abstain from sexual intercourse until they and their partner(s) have been adequately treated (i.e., for 7 days after single-dose therapy or until completion of a 7-day regimen and symptoms resolved). Men who receive a diagnosis of NGU should be tested for HIV and syphilis.
Follow-Up
Men should be provided results of the testing obtained as part of the NGU evaluation, and those with a specific diagnosis of chlamydia, gonorrhea, or trichomonas should be offered partner services and instructed to return 3 months after treatment for repeat testing because of high rates of reinfection, regardless of whether their sex partners were treated (480,481(http://www.cdc.gov/std/tg2015/references.htm#480)) (see Chlamydia, Follow-Up(http://www.cdc.gov/std/tg2015/chlamydia.htm#Follow-Up) and Gonorrhea, Follow-Up(http://www.cdc.gov/std/tg2015/gonorrhea.htm#Follow-Up)).
If symptoms persist or recur after completion of therapy, men should be instructed to return for re-evaluation. Symptoms alone, without documentation of signs or laboratory evidence of urethral inflammation, are not a sufficient basis for retreatment. Providers should be alert to the possible diagnosis of chronic prostatitis/chronic pelvic pain syndrome in men experiencing persistent perineal, penile, or pelvic pain or discomfort, voiding symptoms, pain during or after ejaculation, or new-onset premature ejaculation lasting for >3 months. Men with persistent pain should be referred to a urologist.
Management of Sex Partners
All sex partners of men with NGU within the preceding 60 days should be referred for evaluation, testing, and presumptive treatment with a drug regimen effective against chlamydia. EPT is an alternative approach to treating female partners for CT in the absence of signs and symptoms of PID (95(http://www.cdc.gov/std/tg2015/references.htm#95)). If N. gonorrhea or T. vaginalis is documented, all partners should be evaluated and treated according to the management section for their respective pathogen. To avoid reinfection, sex partners should abstain from sexual intercourse until they and their partner(s) are adequately treated.
Persistent and Recurrent NGU
The objective diagnosis of persistent or recurrent NGU should be made before considering additional antimicrobial therapy. In men who have persistent symptoms after treatment without objective signs of urethral inflammation, the value of extending the duration of antimicrobials has not been demonstrated. Men who have persistent or recurrent NGU can be retreated with the initial regimen if they did not comply with the treatment regimen or were re-exposed to an untreated sex partner.
Recent studies have shown that the most common cause of persistent or recurrent NGU is M. genitalium, especially following doxycycline therapy (277,278(http://www.cdc.gov/std/tg2015/references.htm#277)). Azithromycin 1 g orally in a single dose should be administered to men initially treated with doxycycline. Certain observational studies have shown that moxifloxacin 400 mg orally once daily for 7 days is highly effective against M. genitalium. Therefore, men who fail a regimen of azithromycin should be retreated with moxifloxacin 400 mg orally once daily for 7 days. Higher doses of azithromycin have not been found to be effective for M. genitalium in cases of azithromycin failure (280(http://www.cdc.gov/std/tg2015/references.htm#280)).
T. vaginalis is also known to cause urethritis in men who have sex with women. Although no NAAT for T. vaginalis detection in men has been FDA-cleared in the United States, several large reference laboratories have performed the necessary CLIA validation of a urine-based T. vaginalis NAAT for men for clinical use. Trichomonas NAAT testing is more sensitive than culture (475(http://www.cdc.gov/std/tg2015/references.htm#475)). In areas where T. vaginalis is prevalent, men who have sex with women and have persistent or recurrent urethritis should be presumptively treated with metronidazole 2 g orally in a single dose or tinidazole 2 g orally in a single dose; their partners should be referred for evaluation and appropriate treatment. Persons with persistent or recurrent NGU after presumptive treatment for M. genitalium or T. vaginalis should be referred to a urologist.
Special Considerations
HIV Infection
NGU might facilitate HIV transmission. Persons with NGU and HIV should receive the same treatment regimen as those who are HIV negative
What is bacterial vaginosis?
Bacterial vaginosis (BV)(http://www.cdc.gov/std/bv/default.htm) is an infection caused when too much of certain bacteria change the normal balance of bacteria in the vagina.
How common is bacterial vaginosis?
Bacterial vaginosis is the most common vaginal infection in women ages 15-44.
How is bacterial vaginosis spread?
We do not know about the cause of BV or how some women get it. BV is linked to an imbalance of “good” and “harmful” bacteria that are normally found in a woman's vagina.
We do know that having a new sex partner or multiple sex partners and douching can upset the balance of bacteria in the vagina and put women at increased risk for getting BV.
However, we do not know how sex contributes to BV. BV is not considered an STD, but having BV can increase your chances of getting an STD. BV rarely affects women who have never had sex.
You cannot get BV from toilet seats, bedding, or swimming pools.
How can I avoid getting bacterial vaginosis?
Doctors and scientists do not completely understand how BV is spread, and there are no known best ways to prevent it.
The following basic prevention steps may help lower your risk of developing BV:
- Not having sex;
- Limiting your number of sex partners; and
- Not douching.
I’m pregnant. How does bacterial vaginosis affect my baby?
Pregnant women can get BV. Pregnant women with BV are more likely to have babies who are born premature (early) or with low birth weight than women who do not have BV while pregnant. Low birth weight means having a baby that weighs less than 5.5 pounds at birth.
Treatment is especially important for pregnant women(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm).
How do I know if I have bacterial vaginosis?
Many women with BV do not have symptoms. If you do have symptoms, you may notice a thin white or gray vaginal discharge, odor, pain, itching, or burning in the vagina. Some women have a strong fish-like odor, especially after sex. You may also have burning when urinating; itching around the outside of the vagina, or both.
How will my doctor know if I have bacterial vaginosis?
A health care provider will look at your vagina for signs of BV and perform laboratory tests on a sample of vaginal fluid to determine if BV is present.
Can bacterial vaginosis be cured?
BV will sometimes go away without treatment. But if you have symptoms of BV you should be checked and treated. It is important that you take all of the medicine prescribed to you, even if your symptoms go away. A health care provider can treat BV with antibiotics, but BV can recur even after treatment. Treatment may also reduce the risk for STDs.
Male sex partners of women diagnosed with BV generally do not need to be treated. However, BV may be transferred between female sex partners.
What happens if I don't get treated?
BV can cause some serious health risks, including
- Increasing your chance of getting HIV(http://www.cdc.gov/std/hiv/default.htm) if you have sex with someone who is infected with HIV;
- If you are HIV positive, increasing your chance of passing HIV to your sex partner;
- Making it more likely that you will deliver your baby too early if you have BV while pregnant;
- Increasing your chance of getting other STDs, such as chlamydia(http://www.cdc.gov/std/chlamydia/default.htm) and gonorrhea(http://www.cdc.gov/std/gonorrhea/default.htm). These bacteria can sometimes cause pelvic inflammatory disease (PID)(http://www.cdc.gov/std/pid/stdfact-pid.htm), which can make it difficult or impossible for you to have children.
What is scabies?
Scabies is an infestation of the skin by the human itch mite (Sarcoptes scabiei var. hominis). The microscopic scabies mite burrows into the upper layer of the skin where it lives and lays its eggs. The most common symptoms of scabies are intense itching and a pimple-like skin rash. The scabies mite usually is spread by direct, prolonged, skin-to-skin contact with a person who has scabies.
Scabies is found worldwide and affects people of all races and social classes. Scabies can spread rapidly under crowded conditions where close body and skin contact is frequent. Institutions such as nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Child care facilities also are a common site of scabies infestations.
What is crusted (Norwegian) scabies?
Crusted scabies is a severe form of scabies that can occur in some persons who are immunocompromised (have a weak immune system), elderly, disabled, or debilitated. It is also called Norwegian scabies. Persons with crusted scabies have thick crusts of skin that contain large numbers of scabies mites and eggs. Persons with crusted scabies are very contagious to other persons and can spread the infestation easily both by direct skin-to-skin contact and by contamination of items such as their clothing, bedding, and furniture. Persons with crusted scabies may not show the usually signs and symptoms of scabies such as the characteristic rash or itching (pruritus). Persons with crusted scabies should receive quick and aggressive medical treatment for their infestation to prevent outbreaks of scabies.
How soon after infestation do symptoms of scabies begin?
If a person has never had scabies before, symptoms may take as long as 4-6 weeks to begin. It is important to remember that an infested person can spread scabies during this time, even if he/she does not have symptoms yet.
In a person who has had scabies before, symptoms usually appear much sooner (1-4 days) after exposure.
What are the signs and symptoms of scabies infestation?
The most common signs and symptoms of scabies are intense itching (pruritus), especially at night, and a pimple-like (papular) itchy rash. The itching and rash each may affect much of the body or be limited to common sites such as the wrist, elbow, armpit, webbing between the fingers, nipple, penis, waist, belt-line, and buttocks. The rash also can include tiny blisters (vesicles) and scales. Scratching the rash can cause skin sores; sometimes these sores become infected by bacteria.
Tiny burrows sometimes are seen on the skin; these are caused by the female scabies mite tunneling just beneath the surface of the skin. These burrows appear as tiny raised and crooked (serpiginous) grayish-white or skin-colored lines on the skin surface. Because mites are often few in number (only 10-15 mites per person), these burrows may be difficult to find. They are found most often in the webbing between the fingers, in the skin folds on the wrist, elbow, or knee, and on the penis, breast, or shoulder blades.
The head, face, neck, palms, and soles often are involved in infants and very young children, but usually not adults and older children.
Persons with crusted scabies may not show the usual signs and symptoms of scabies such as the characteristic rash or itching (pruritus).
How did I get scabies?
Scabies usually is spread by direct, prolonged, skin-to-skin contact with a person who has scabies. Contact generally must be prolonged; a quick handshake or hug usually will not spread scabies. Scabies is spread easily to sexual partners and household members. Scabies in adults frequently is sexually acquired. Scabies sometimes is spread indirectly by sharing articles such as clothing, towels, or bedding used by an infested person; however, such indirect spread can occur much more easily when the infested person has crusted scabies.
How is scabies infestation diagnosed?
Diagnosis of a scabies infestation usually is made based on the customary appearance and distribution of the rash and the presence of burrows. Whenever possible, the diagnosis of scabies should be confirmed by identifying the mite, mite eggs, or mite fecal matter (scybala). This can be done by carefully removing a mite from the end of its burrow using the tip of a needle or by obtaining skin scraping to examine under a microscope for mites, eggs, or mite fecal matter. It is important to remember that a person can still be infested even if mites, eggs, or fecal matter cannot be found; typically fewer than 10-15 mites can be present on the entire body of an infested person who is otherwise healthy. However, persons with crusted scabies can be infested with thousands of mites and should be considered highly contagious.
How long can scabies mites live?
On a person, scabies mites can live for as long as 1-2 months. Off a person, scabies mites usually do not survive more than 48-72 hours. Scabies mites will die if exposed to a temperature of 50°C (122°F) for 10 minutes.
Can scabies be treated?
Yes. Products used to treat scabies are called scabicides because they kill scabies mites; some also kill eggs. Scabicides to treat human scabies are available only with a doctor’s prescription; no "over-the-counter" (non-prescription) products have been tested and approved for humans.
Always follow carefully the instructions provided by the doctor and pharmacist, as well as those contained in the box or printed on the label. When treating adults and older children, scabicide cream or lotion is applied to all areas of the body from the neck down to the feet and toes; when treating infants and young children, the cream or lotion also is applied to the head and neck. The medication should be left on the body for the recommended time before it is washed off. Clean clothes should be worn after treatment.
In addition to the infested person, treatment also is recommended for household members and sexual contacts, particularly those who have had prolonged skin-to-skin contact with the infested person. All persons should be treated at the same time in order to prevent reinfestation. Retreatment may be necessary if itching continues more than 2-4 weeks after treatment or if new burrows or rash continue to appear.
Never use a scabicide intended for veterinary or agricultural use to treat humans!
Who should be treated for scabies?
Anyone who is diagnosed with scabies, as well as his or her sexual partners and other contacts who have had prolonged skin-to-skin contact with the infested person, should be treated. Treatment is recommended for members of the same household as the person with scabies, particularly those persons who have had prolonged skin-to-skin contact with the infested person. All persons should be treated at the same time to prevent reinfestation.
Retreatment may be necessary if itching continues more than 2-4 weeks after treatment or if new burrows or rash continue to appear.
How soon after treatment will I feel better?
If itching continues more than 2-4 weeks after initial treatment or if new burrows or rash continue to appear (if initial treatment includes more than one application or dose, then the 2-4 time period begins after the last application or dose), retreatment with scabicide may be necessary; seek the advice of a physician.
Did I get scabies from my pet?
No. Animals do not spread human scabies. Pets can become infested with a different kind of scabies mite that does not survive or reproduce on humans but causes "mange" in animals. If an animal with "mange" has close contact with a person, the animal mite can get under the person’s skin and cause temporary itching and skin irritation. However, the animal mite cannot reproduce on a person and will die on its own in a couple of days. Although the person does not need to be treated, the animal should be treated because its mites can continue to burrow into the person’s skin and cause symptoms until the animal has been treated successfully.
Can scabies be spread by swimming in a public pool?
Scabies is spread by prolonged skin-to-skin contact with a person who has scabies. Scabies sometimes also can be spread by contact with items such as clothing, bedding, or towels that have been used by a person with scabies, but such spread is very uncommon unless the infested person has crusted scabies.
Scabies is very unlikely to be spread by water in a swimming pool. Except for a person with crusted scabies, only about 10-15 scabies mites are present on an infested person; it is extremely unlikely that any would emerge from under wet skin.
Although uncommon, scabies can be spread by sharing a towel or item of clothing that has been used by a person with scabies.
How can I remove scabies mites from my house or carpet?
Scabies mites do not survive more than 2-3 days away from human skin. Items such as bedding, clothing, and towels used by a person with scabies can be decontaminated by machine-washing in hot water and drying using the hot cycle or by dry-cleaning. Items that cannot be washed or dry-cleaned can be decontaminated by removing from any body contact for at least 72 hours.
Because persons with crusted scabies are considered very infectious, careful vacuuming of furniture and carpets in rooms used by these persons is recommended.
Fumigation of living areas is unnecessary.
How can I remove scabies mites from my clothes?
Scabies mites do not survive more than 2-3 days away from human skin. Items such as bedding, clothing, and towels used by a person with scabies can be decontaminated by machine-washing in hot water and drying using the hot cycle or by dry-cleaning. Items that cannot be washed or dry-cleaned can be decontaminated by removing from any body contact for at least 72 hours.
My spouse and I were diagnosed with scabies. After several treatments, he/she still has symptoms while I am cured. Why?
The rash and itching of scabies can persist for several weeks to a month after treatment, even if the treatment was successful and all the mites and eggs have been killed. Your health care provider may prescribe additional medication to relieve itching if it is severe. Symptoms that persist for longer than 2 weeks after treatment can be due to a number of reasons, including:
- Incorrect diagnosis of scabies. Many drug reactions can mimic the symptoms of scabies and cause a skin rash and itching; the diagnosis of scabies should be confirmed by a skin scraping that includes observing the mite, eggs, or mite feces (scybala) under a microscope. If you are sleeping in the same bed with your spouse and have not become reinfested, and you have not retreated yourself for at least 30 days, then it is unlikely that your spouse has scabies.
- Reinfestation with scabies from a family member or other infested person if all patients and their contacts are not treated at the same time; infested persons and their contacts must be treated at the same time to prevent reinfestation.
- Treatment failure caused by resistance to medication, by faulty application of topical scabicides, or by failure to do a second application when necessary; no new burrows should appear 24-48 hours after effective treatment.
- Treatment failure of crusted scabies because of poor penetration of scabicide into thick scaly skin containing large numbers of scabies mites; repeated treatment with a combination of both topical and oral medication may be necessary to treat crusted scabies successfully.
- Reinfestation from items (fomites) such as clothing, bedding, or towels that were not appropriately washed or dry-cleaned (this is mainly of concern for items used by persons with crusted scabies); potentially contaminated items (fomites) should be machine washed in hot water and dried using the hot temperature cycle, dry-cleaned, or removed from skin contact for at least 72 hours.
- An allergic skin rash (dermatitis); or
- Exposure to household mites that cause symptoms to persist because of cross-reactivity between mite antigens.
If itching continues more than 2-4 weeks or if new burrows or rash continue to appear, seek the advice of a physician; retreatment with the same or a different scabicide may be necessary.
If I come in contact with a person who has scabies, should I treat myself?
No. If a person thinks he or she might have scabies, he/she should contact a doctor. The doctor can examine the person, confirm the diagnosis of scabies, and prescribe an appropriate treatment. Products used to treat scabies in humans are available only with a doctor’s prescription.
Sleeping with or having sex with any scabies infested person presents a high risk for transmission. The longer a person has skin-to-skin exposure, the greater is the likelihood for transmission to occur. Although briefly shaking hands with a person who has non-crusted scabies could be considered as presenting a relatively low risk, holding the hand of a person with scabies for 5-10 minutes could be considered to present a relatively high risk of transmission. However, transmission can occur even after brief skin-to-skin contact, such as a handshake, with a person who has crusted scabies. In general, a person who has skin-to-skin contact with a person who has crusted scabies would be considered a good candidate for treatment.
To determine when prophylactic treatment should be given to reduce the risk of transmission, early consultation should be sought with a health care provider who understands:
- the type of scabies (i.e. non-crusted vs crusted) to which a person has been exposed;
- the degree and duration of skin exposure that a person has had to the infested patient;
- whether the exposure occurred before or after the patient was treated for scabies; and,
- whether the exposed person works in an environment where he/she would be likely to expose other people during the asymptomatic incubation period. For example, a nurse or caretaker who works in a nursing home or hospital often would be treated prophylactically to reduce the risk of further scabies transmission in the facility.
What is PID?
Pelvic inflammatory disease is an infection of a woman’s reproductive organs. It is a complication often caused by some STDs, like chlamydia(http://www.cdc.gov/std/chlamydia/default.htm) and gonorrhea(http://www.cdc.gov/std/gonorrhea/default.htm). Other infections that are not sexually transmitted can also cause PID.
How do I get PID?
You are more likely to get PID if you
- Have an STD and do not get treated;
- Have more than one sex partner;
- Have a sex partner who has sex partners other than you;
- Have had PID before;
- Are sexually active and are age 25 or younger;
- Douche;
- Use an intrauterine device (IUD) for birth control.
How can I reduce my risk of getting PID?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting PID:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
How do I know if I have PID?
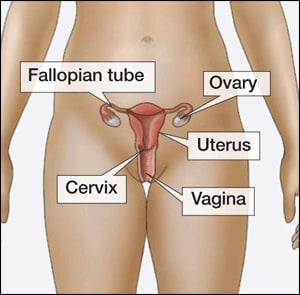 There are no tests for PID. A diagnosis is usually based on a combination of your medical history, physical exam, and other test results. You may not realize you have PID because your symptoms may be mild, or you may not experience any symptoms. However, if you do have symptoms, you may notice
There are no tests for PID. A diagnosis is usually based on a combination of your medical history, physical exam, and other test results. You may not realize you have PID because your symptoms may be mild, or you may not experience any symptoms. However, if you do have symptoms, you may notice
- Pain in your lower abdomen;
- Fever;
- An unusual discharge with a bad odor from your vagina;
- Pain and/or bleeding when you have sex;
- Burning sensation when you urinate; or
- Bleeding between periods.
You should
- Be examined by your doctor if you notice any of these symptoms;
- Promptly see a doctor if you think you or your sex partner(s) have or were exposed to an STD;
- Promptly see a doctor if you have any genital symptoms such as an unusual sore, a smelly discharge, burning when peeing, or bleeding between periods;
- Get a test for chlamydia every year if you are sexually active and 25 years of age or younger;
- Have an honest and open talk with your health care provider if you are sexually active and ask whether you should be tested for other STDs.
Can PID be cured?
Yes, if PID is diagnosed early, it can be treated. However, treatment won’t undo any damage that has already happened to your reproductive system. The longer you wait to get treated, the more likely it is that you will have complications from PID. While taking antibiotics, your symptoms may go away before the infection is cured. Even if symptoms go away, you should finish taking all of your medicine. Be sure to tell your recent sex partner(s), so they can get tested and treated for STDs, too. It is also very important that you and your partner both finish your treatment before having any kind of sex so that you don’t re-infect each other.
You can get PID again if you get infected with an STD again. Also, if you have had PID before, you have a higher chance of getting it again.
What happens if I don't get treated?
If diagnosed and treated early, the complications of PID can be prevented. Some of the complications of PID are
- Formation of scar tissue both outside and inside the fallopian tubes that can lead to tubal blockage;
- Ectopic pregnancy (pregnancy outside the womb);
- Infertility (inability to get pregnant);
- Long-term pelvic/abdominal pain.
Lice are parasitic insects that can be found on people's heads, and bodies, including the pubic area. Human lice survive by feeding on human blood. Lice found on each area of the body are different from each other. The three types of lice that live on humans are:
- Pediculus humanus capitis (head louse),
- Pediculus humanus corporis (body louse, clothes louse), and
- Pthirus pubis ("crab" louse, pubic louse).
Only the body louse is known to spread disease.
Lice infestations (pediculosis and pthiriasis) are spread most commonly by close person-to-person contact. Dogs, cats, and other pets do not play a role in the transmission of human lice. Lice move by crawling; they cannot hop or fly. Both over-the-counter and prescription medications are available for treatment of lice infestations.
Pubic
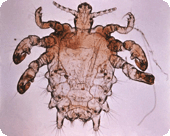
Adult pubic lice are 1.1–1.8 mm in length. Pubic lice typically are found attached to hair in the pubic area but sometimes are found on coarse hair elsewhere on the body (for example, eyebrows, eyelashes, beard, mustache, chest, armpits, etc.).
What is trichomoniasis?
Trichomoniasis(http://www.cdc.gov/std/trichomonas/default.htm) (or “trich”) is a very common sexually transmitted disease (STD) that is caused by infection with a protozoan parasite called Trichomonas vaginalis. Although symptoms of the disease vary, most women and men who have the parasite cannot tell they are infected.
How common is trichomoniasis?
Trichomoniasis is considered the most common curable STD. In the United States, an estimated 3.7 million people have the infection, but only about 30% develop any symptoms of trichomoniasis. Infection is more common in women than in men, and older women are more likely than younger women to have been infected.
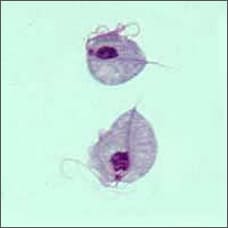
Two Trichomonas vaginalis parasites, magnified (seen under a microscope)
How do people get trichomoniasis?
The parasite is passed from an infected person to an uninfected person during sex. In women, the most commonly infected part of the body is the lower genital tract (vulva, vagina, or urethra), and in men, the most commonly infected body part is the inside of the penis (urethra). During sex, the parasite is usually transmitted from a penis to a vagina, or from a vagina to a penis, but it can also be passed from a vagina to another vagina. It is not common for the parasite to infect other body parts, like the hands, mouth, or anus. It is unclear why some people with the infection get symptoms while others do not, but it probably depends on factors like the person’s age and overall health. Infected people without symptoms can still pass the infection on to others.
What are the signs and symptoms of trichomoniasis?
About 70% of infected people do not have any signs or symptoms. When trichomoniasis does cause symptoms, they can range from mild irritation to severe inflammation. Some people with symptoms get them within 5 to 28 days after being infected, but others do not develop symptoms until much later. Symptoms can come and go.
Men with trichomoniasis may feel itching or irritation inside the penis, burning after urination or ejaculation, or some discharge from the penis.
Women with trichomoniasis may notice itching, burning, redness or soreness of the genitals, discomfort with urination, or a thin discharge with an unusual smell that can be clear, white, yellowish, or greenish.
Having trichomoniasis can make it feel unpleasant to have sex. Without treatment, the infection can last for months or even years.
What are the complications of trichomoniasis?
Trichomoniasis can increase the risk of getting or spreading other sexually transmitted infections. For example, trichomoniasis can cause genital inflammation that makes it easier to get infected with the HIV virus(http://www.cdc.gov/std/hiv), or to pass the HIV virus on to a sex partner.
How does trichomoniasis affect a pregnant woman and her baby?
Pregnant women with trichomoniasis(http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm) are more likely to have their babies too early (preterm delivery). Also, babies born to infected mothers are more likely to have an officially low birth weight (less than 5.5 pounds).
How is trichomoniasis diagnosed?
It is not possible to diagnose trichomoniasis based on symptoms alone. For both men and women, your primary care doctor or another trusted health care provider must do a check and a laboratory test to diagnose this infection.
What is the treatment for trichomoniasis?
Trichomoniasis can be cured with a single dose of prescription antibiotic medication (either metronidazole or tinidazole), pills which can be taken by mouth. It is okay for pregnant women to take this medication. Some people who drink alcohol within 24 hours after taking this kind of antibiotic can have uncomfortable side effects.
People who have been treated for trichomoniasis can get it again. About 1 in 5 people get infected again within 3 months after treatment. To avoid getting reinfected, make sure that all of your sex partners get treated too, and wait to have sex again until all of your symptoms go away (about a week). Get checked again if your symptoms come back.
How can trichomoniasis be prevented?
Using latex condoms correctly every time you have sex will help reduce the risk of getting or spreading trichomoniasis. However, condoms don’t cover everything, and it is possible to get or spread this infection even when using a condom.
The only sure way to prevent sexually transmitted infections is to avoid having sex entirely. Another approach is to talk about these kinds of infections before you have sex with a new partner, so that you can make informed choices about the level of risk you are comfortable taking with your sex life.
If you or someone you know has questions about trichomoniasis or any other STD, especially with symptoms like unusual discharge, burning during urination, or a sore in the genital area, check in with a health care provider and get some answers